Radiation oncology is a medical specialty that uses high-energy radiation to treat cancer. It involves the careful planning, delivery, and monitoring of radiation therapy to destroy cancer cells, shrink tumors, and relieve symptoms. Radiation therapy can be used alone or in combination with other treatments like surgery, chemotherapy, or immunotherapy, depending on the type, location, and stage of cancer.
The goal of radiation oncology is to target the tumor while minimizing damage to surrounding healthy tissue. This requires highly specialized equipment, expertise in radiation physics, and precise treatment planning. Radiation oncologists work closely with medical physicists, dosimetrists, radiation therapists, and other healthcare professionals to deliver the most effective treatment while managing potential side effects.
- Types of Radiation Therapy
There are several forms of radiation therapy used in oncology, each with its own advantages, depending on the type of cancer and its location. The main types include:
1.1. External Beam Radiation Therapy (EBRT)
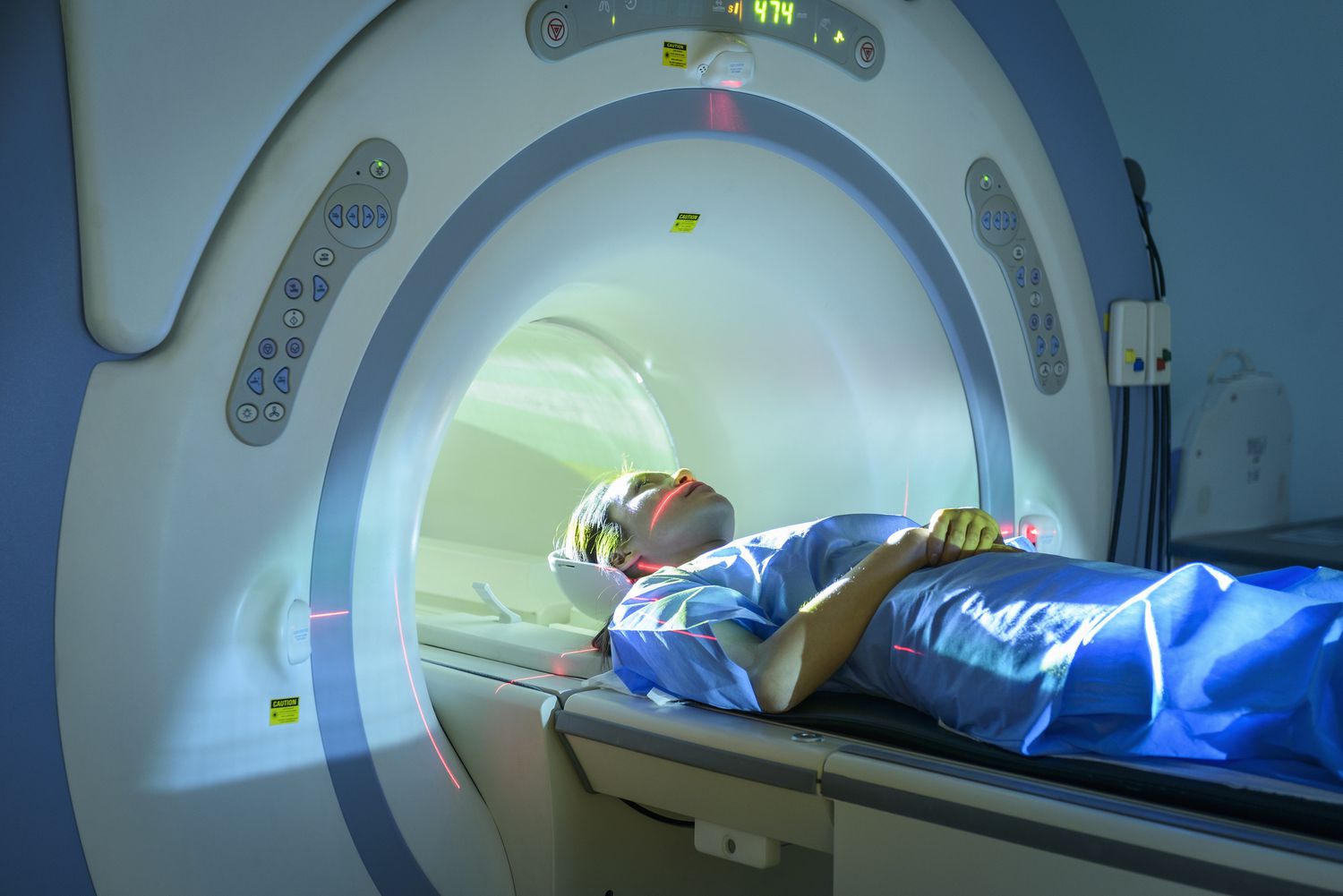
External beam radiation therapy (EBRT) is the most common form of radiation therapy and involves directing high-energy beams of radiation from outside the body to the cancerous tumor.
Technique: The patient typically lies on a treatment table, and a machine called a linear accelerator (linac) is used to deliver radiation. The machine can rotate around the patient to target the tumor from various angles, ensuring the tumor receives the optimal dose while minimizing exposure to healthy tissues.
Indications: EBRT is used for cancers that are localized to a specific area, such as breast, prostate, lung, or brain cancers. It is also often used in combination with surgery or chemotherapy to shrink tumors or treat residual cancer cells.
Specialized Types of External Beam Radiation Therapy:
Three-Dimensional Conformal Radiation Therapy (3D-CRT): This technique uses imaging scans (CT or MRI) to map the shape of the tumor in three dimensions. The radiation beams are shaped to match the tumor’s contour, allowing for precise targeting.
Intensity-Modulated Radiation Therapy (IMRT): IMRT is an advanced form of 3D-CRT that allows for the modulation (adjustment) of the intensity of radiation beams. It enables the delivery of higher radiation doses to the tumor while sparing nearby healthy tissues.
Image-Guided Radiation Therapy (IGRT): This technique uses imaging technologies, like CT or X-ray, to guide the delivery of radiation during each treatment session. It ensures the tumor is targeted accurately, especially if it shifts or changes position.
Stereotactic Body Radiation Therapy (SBRT): SBRT delivers very high doses of radiation to small, well-defined tumors with high precision, typically in 1 to 5 sessions. It is commonly used for cancers in the lungs, liver, and spine.
Stereotactic Radiosurgery (SRS): This is a specialized form of SBRT used to treat tumors in the brain. It delivers highly focused radiation to a very small area, allowing for the treatment of brain tumors without the need for traditional surgery.
1.2. Internal Radiation Therapy (Brachytherapy)
Brachytherapy involves placing a radioactive source directly inside or very close to the tumor. It is commonly used to treat cancers of the prostate, cervix, and uterus, as well as certain head and neck cancers.
Technique: Radioactive seeds or sources are placed inside the body using thin tubes, needles, or applicators. These sources emit radiation over a period of time, targeting the cancer from within. This allows for a higher concentration of radiation to be delivered directly to the tumor while minimizing damage to nearby healthy tissues.
Types of Brachytherapy:
Prostate Brachytherapy: Tiny radioactive seeds are implanted into the prostate to treat prostate cancer. This is typically used for localized prostate cancer.
Gynecologic Brachytherapy: Radioactive sources are placed in the vagina or cervix for cancers of the cervix or uterus.
Head and Neck Brachytherapy: In certain cases, radioactive sources are placed within the tumor or close to it to treat cancers in the head and neck area.
1.3. Systemic Radiation Therapy
Systemic radiation therapy uses radioactive substances that are either swallowed or injected into the bloodstream to target cancer cells throughout the body. The most common example is radioactive iodine therapy (I-131), which is used to treat thyroid cancer.
Procedure: The radioactive substance is absorbed by the cancerous cells, delivering radiation directly to the tumor while minimizing exposure to normal tissues.
Applications:
Thyroid Cancer: I-131 is used to treat both hyperthyroidism and thyroid cancer, particularly to destroy residual thyroid tissue after surgery.
Bone Pain: Certain forms of radiation, like radium-223, can be used to treat bone metastases, relieving pain and reducing the risk of fractures.
1.4. Proton Therapy
Proton therapy is a specialized form of radiation therapy that uses protons (charged particles) rather than X-rays to treat cancer. Protons can be precisely controlled to deposit their energy directly at the tumor site, minimizing damage to surrounding healthy tissues.
Advantages: Proton therapy is particularly useful for treating tumors near critical structures, such as in pediatric patients, brain tumors, and tumors in the spine or eye.
Limitations: Proton therapy requires specialized equipment and is more costly than conventional radiation therapy, limiting its availability.
- Indications for Radiation Therapy
Radiation therapy is used to treat a wide variety of cancers, both curative and palliative. The key indications include:
Curative Treatment: For localized cancers or tumors that are amenable to radiation, such as breast cancer, prostate cancer, and some head and neck cancers. Radiation may be used to shrink tumors before surgery, destroy remaining cancer cells after surgery, or to treat tumors that cannot be surgically removed.
Adjuvant Therapy: Radiation may be used after surgery to kill any remaining cancer cells and reduce the risk of cancer recurrence. For example, after breast-conserving surgery (lumpectomy), radiation is often given to reduce the risk of recurrence in the breast.
Neoadjuvant Therapy: Radiation may be given before surgery to shrink a tumor, making it easier to remove. This approach is often used for cancers of the rectum, bladder, or head and neck.
Palliative Treatment: In advanced cancers, radiation can be used to shrink tumors and relieve symptoms such as pain, bleeding, and obstruction. For example, it is commonly used to treat bone metastases, brain metastases, or to relieve airway obstruction from lung cancer.
- How Radiation Therapy Works
Radiation therapy works by damaging the DNA inside cells, which prevents them from growing or dividing. While normal cells can repair this damage, cancer cells, which are dividing rapidly, are more likely to accumulate DNA damage and die as a result. There are two primary mechanisms through which radiation affects cancer cells:
3.1. Direct Effect
Radiation directly damages the DNA within cancer cells, causing double-strand breaks that the cell cannot repair. This damage leads to cell death.
3.2. Indirect Effect
Radiation also creates free radicals and other reactive oxygen species that damage the DNA. These free radicals are produced by radiation interacting with water molecules in the body, and they indirectly harm the cancer cells.
Both effects ultimately result in the death of cancer cells or their inability to reproduce, which leads to tumor shrinkage or elimination.
- Radiation Therapy Planning and Delivery
One of the most important aspects of radiation oncology is treatment planning, which ensures that the radiation is precisely targeted to the tumor and minimizes exposure to healthy tissue. This process involves:
4.1. Simulation
Before treatment, patients undergo a simulation to plan the exact position and angles from which radiation will be delivered. The process may include:
Imaging: CT scans, MRI, or PET scans are performed to precisely locate the tumor and map its size, shape, and position relative to surrounding tissues.
Marking the Skin: Small, permanent or semi-permanent marks may be placed on the skin to guide the patient’s positioning during each treatment session.
4.2. Treatment Planning
Once the simulation is complete, the radiation oncologist, in collaboration with medical physicists and dosimetrists, creates a detailed radiation treatment plan. This plan determines:
The dosage of radiation to be delivered.
The exact angles and positions of the radiation beams.
The treatment duration and number of sessions (e.g., daily treatments for 5–7 weeks).
4.3. Treatment Delivery
Radiation therapy sessions are typically scheduled over several weeks, with each treatment lasting only a few minutes. The patient may be positioned on the treatment table using immobilization devices to ensure accurate delivery.
External Beam Radiation: Radiation is delivered through the skin, using a machine (like a linear accelerator). The patient lies still while the machine rotates around them to deliver radiation from multiple angles.
Internal Radiation (Brachytherapy): In the case of brachytherapy, radioactive sources are inserted into or near the tumor.
4.4. Monitoring During Treatment
During the course of treatment, the radiation oncologist will regularly monitor the patient for any side effects and adjust the treatment if necessary. Imaging may be performed periodically to ensure that the tumor is being targeted accurately and to check for changes in tumor size.
- Side Effects of Radiation Therapy
While radiation therapy is highly effective in treating cancer, it can cause side effects due to the damage to normal healthy cells surrounding the tumor. The severity and type of side effects depend on the area being treated, the radiation dose, and the patient's overall health.
Common Side Effects:
- Fatigue: A common and often persistent side effect of radiation therapy, which may last for weeks or months after treatment.
- Skin Irritation: Skin in the treated area may become red, dry, or itchy, similar to a sunburn.
- Hair Loss: Hair loss can occur in the area being treated, such as the scalp or face, but typically regrows after treatment.
- Gastrointestinal Issues: Radiation to the abdomen, pelvis, or bowel can cause nausea, diarrhea, or bowel discomfort.
- Urinary and Sexual Dysfunction: Radiation to the pelvic region (e.g., for prostate or gynecological cancers) can cause urinary frequency, incontinence, or sexual dysfunction.
- Long-Term Side Effects:
- Fibrosis: Scarring and thickening of tissues in the irradiated area, which can cause stiffness and discomfort.
- Secondary Cancers: Radiation therapy can increase the risk of developing a second cancer many years after treatment, although the risk is relatively low compared to the benefits of tumor control.
- Radiation oncologists carefully consider these side effects during treatment planning and take measures to minimize harm to healthy tissues, such as using advanced techniques like IMRT, proton therapy, or brachytherapy.
- Conclusion
Radiation oncology is a powerful and essential tool in the fight against cancer. With modern advancements in imaging, treatment planning, and delivery techniques, radiation therapy is increasingly precise, minimizing harm to healthy tissues while maximizing the impact on cancer cells. While side effects can occur, careful planning and advanced technologies allow radiation oncologists to provide highly effective treatment with a focus on quality of life and overall survival. As part of a multidisciplinary cancer treatment plan, radiation oncology plays a critical role in improving outcomes for cancer patients.